
Meet the wellness trends reshaping mental health care in the UK: from prevention-first thinking and digital support to neuroscience and progressive therapy.
As surgery became popular in the 19th century, boosted by the development of anesthesia and implementation of antisepsis, mental healthcare and mental wellness are peaking right now due to increased affordability, variety of digital tools, and progressive therapy. However, poor mental health still costs roughly £150 billion a year to the UK economy. The hope for the nation’s well-being is in the latest trends that focus on integration, neuroscience, innovative treatments, and lifestyle changes.
Trend #1 – Preventive and Holistic Approaches
In 2025, many of us are more in touch with our minds and try to calm even ripples of mental distress long before psychosis or other mental collapses come. It’s easier to keep from falling apart than to glue everything back together.
Being aware is almost a synonym of being healthy. Understanding the moment when stress or anxiety starts to boil is crucial to know when we need first aid. That’s why, in schools, children and teens explore how to recognise emotions, while their parents follow mental health influencers to learn the same.
We are predictable. Research teams can read early red flags in everyday behaviour, when someone stops leaving the house, scrolls through the night, or suddenly withdraws from chats, and use them to find treatment before a crisis hits.
United we stand. In a 2025 survey by the British Association for Counselling & Psychotherapy, 72% of 16–25-year-olds said loneliness can trigger mental health problems, and open conversations with friends, family, or support groups are among the best investments in mental well-being.
Emotional-literacy learning, the value we place on human connections, and even how we use our phones all point to a shift toward proactive care that integrates physical, emotional, and social health.
Trend #2 – Technology and Digital Wellness
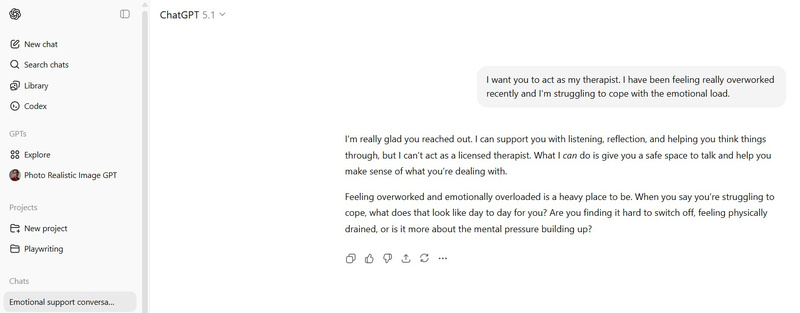
Gen Z behaviour and viral posts on Reddit show how tools like ChatGPT can replace pricey therapists, apps can track our emotions, and things that 10 years ago could only be monitored in clinics now sit in tiny gadgets on our wrists.
From the therapist’s office to online consultations to AI. Mental health support keeps evolving with technologies like AI-powered apps that offer reflective conversations, personalized mindfulness exercises, and cognitive-behavioural techniques. The NHS has already explicitly warned young people not to use general chatbots like ChatGPT as substitutes for therapy. Yet globally, the mental-health apps market is worth around £6–7 billion, and most forecasts expect it to grow to roughly £13–15 billion by 2030.
Meet your fears safely. Exposure therapy used to mean sitting in a therapist’s office, imagining feared situations, or slowly facing them in real life. Nowadays, it is increasingly moving onto virtual reality platforms as a safe way to help people overcome phobias, PTSD, and anxiety.
Apps to help avoid relapse. In a 2025 cross-sectional study of people in treatment, 45% said they’d used an app or website to support their recovery. Another study of outpatients found that 70.1% would use a relapse-prevention app, and 72.3% would also be interested in relapse-prevention text messages.
In the future, digital support will be cheaper and reach more people, but it raises questions about privacy, effectiveness, and oversight. Making digital mental health safe and reliable will require engineers, clinicians, and regulators to collaborate.
Trend #3 – Neuroscience and the Biology of Well‑Being
Fortunately, the phrase “you can’t teach an old dog new tricks” doesn’t apply to the human brain. Thanks to neuroplasticity, we can reorganise ourselves by forming new connections whenever we learn something, have a new experience, exercise, or even sit still in meditation. And if we want our mind to do a good job, it needs good care, that’s where the gut comes in.
Life is in motion. When we move, the brain releases more brain-derived neurotrophic factor, a kind of growth support for neurons that helps them stay alive, connect and even regenerate. Over time, it can steady mood, ease symptoms of depression and anxiety, sharpen memory and attention, and directly support neuroplasticity.
Don’t worry, be mindful. 2025 reviews show the mind–body practices like meditation, yoga, and breathwork activate the parasympathetic nervous system, and make it easier for the brain to rewire, which is why now you see them built into many wellness programmes.
We are what we eat. Nutritional psychiatry is a fast-growing field that explores the gut–brain axis. Understanding how inflammation, gut microbes, and genes influence mental health helps clinicians treat the mind and body together.
Neuroscience now offers hard evidence for practices once dismissed as mystical, and for everyday activities we never used to connect with mental health. Now you know that well-being is flexible, and it’s not just in your head, it’s also in your muscles and microbiome.
Trend #4 – Progressive Mental Health Solutions

Mental wealth is no longer just personal, it’s becoming a common wealth. Integrative ways to feel better replace the old one-service approach, and therapy looks like a smart network of digital and human support. In many modern services, it starts with a quick online check-in and a few digital tools, then, if that’s not enough, moves into structured therapy and changes to daily habits.
Another look at trauma. Instead of endlessly retelling the story, approaches like eye movement desensitisation and reprocessing, EMDR, and body-based trauma work give people a more contained way to deal with what happened. In EMDR, you briefly touch the memory while your attention is pulled left–right by fingers, lights, or taps, so the experience can be replayed without overwhelming the system. Somatic methods stay close to what the body is doing, clenched jaw, shallow breath, buzzing chest, and help those reactions complete and settle, so the nervous system isn’t stuck in permanent alarm mode.
It’s teamwork. Recent collaborative-care studies show people do better with depression and anxiety when their general practitioner, mental-health clinician, and care coordinator work from the same plan instead of in separate bubbles.
Communities as new institutions. Following WHO’s 2025 direction, more attention is going to services based in neighbourhoods, schools, and workplaces, rather than locking everything away in hospitals.
We can expect mental health care to be more flexible, collaborative, and far more personalised. If you want to see where it’s heading in real life, not just in glossy reports or out-of-touch studies, dive into the experiments, insights from human stories, and future-facing ideas at https://statesofmind.com/
Trend #5 – The Workplace and the New Definition of Well‑Being
Work still takes a big part of life. Global estimates suggest we’ll spend around 70,000–90,000 hours on the job, roughly a third of our waking adult life. So it’s no surprise that the office, or the kitchen table for many remote workers, has become one of the main battlegrounds for mental health.
More organisations have a plan, not just a poster. In the UK, the share of employers with a stand-alone wellbeing strategy has gone from 44% in 2020 to 57% in 2025. That means it’s no longer only big corporations talking about mental health on slide decks, mid-sized companies, charities, and public-sector teams are putting real policies in place around stress, burnout, workload, and support, instead of relying on a token wellness week.
Health before deadlines. Roughly 74% of UK organisations say employee wellbeing is something senior leaders actively pay attention to. Employers are learning that support only works if people can actually use it, so they offer counselling or employee assistance programmes, signpost to mental-health first aiders, and build in flexible work patterns for people with long-term conditions, caring responsibilities, or ongoing therapy.
From classrooms to boardrooms, mental wellness is shifting from reaction to prevention. The digital mental health market is booming, with 2025 analyses estimating it at roughly £26 billion globally and forecasting it will climb to well over £120 billion by 2034, which offers 24/7 support but demands strong privacy safeguards. Neuroscience highlights how regular physical exercise and long-standing practices such as mindfulness and yoga can support mood, cognition, and brain plasticity.
Data-driven care, nutritional psychiatry, community programmes, and cautiously emerging new treatments are creating mind-and-body-focused paths to healing. Taken together, these trends suggest a future where science and innovation make mental wellness proactive, personalised, and fully integrated into everyday life.
